STICHES: Coronary Bypass Surgery in Patients with Left Ventricular Dysfunction The STICH Extension Study (STICHES) now published in the New England Journal of Medicine has reported on nearly ten years of follow-up from the original study. Over the extended follow-up period a significant survival benefit was seen in the group randomised to medical therapy plus
STICHES: Coronary Bypass Surgery in Patients with Left Ventricular Dysfunction
The STICH Extension Study (STICHES) now published in the New England Journal of Medicine has reported on nearly ten years of follow-up from the original study. Over the extended follow-up period a significant survival benefit was seen in the group randomised to medical therapy plus CABG. Rate of death was 16% lower in those assigned to surgical treatment with an absolute difference at 10 years on Kaplan-Meier analysis of 8%.
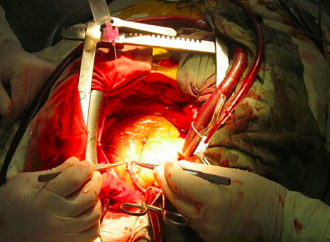
Ischaemic heart disease is the most common cause of heart failure in the industrialised world. Whilst the role of coronary artery bypass grafting (CABG) in angina is established, the role of revascularisation for ischaemic cardiomyopathy is not clear. Landmark CABG trials conducted in the 1970s and ‘80s excluded patients with severe left ventricular systolic dysfunction (LVSD) and few patients had a heart failure syndrome [1-3]. Whilst these important early studies demonstrated the safety of CABG, a survival advantage in those with either normal or impaired (LVEF 40-50%) left ventricular function was not seen. Though there are clear theoretical benefits in restoring blood flow to dysfunctional myocardium, assuming that myocardial injury is not irreversible, there were no randomised data to support this hypothesis.
The ‘Surgical Treatment for Ischaemic Heart Failure’ (STICH) [4] study was conducted to determine if medical therapy plus surgical revascularisation versus medical therapy alone would offer a survival advantage in ischaemic cardiomyopathy with severe left ventricular systolic impairment (LVEF <35%). The five year results of the study did not find survival benefit with CABG (HR 0.86, 95% confidence interval 0.72-1.04, p=0.12). The early mortality in the CABG arm probably outweighed an apparent late survival benefit. However, as an intention to treat analysis treatment arm crossover rates of 17% may have obscured potential survival benefit of CABG.
The STICH Extension Study (STICHES) [5] now published in the New England Journal of Medicine has reported on nearly ten years of follow-up from the original study. Over the extended follow-up period a significant survival benefit was seen in the group randomised to medical therapy plus CABG. Rate of death was 16% lower in those assigned to surgical treatment with an absolute difference at 10 years on Kaplan-Meier analysis of 8%. Median survival in those assigned to surgical revascularisation was 7.73 vs 6.29 years in the medical arm demonstrating that with sufficient time the surgical risk of CABG, in this study 3.6% at 30 days, is more than offset by ten years. Therefore providing compelling evidence that patients with severe LVSD and coronary disease amenable to surgical revascularisation should now be offered CABG.
However an important caveat is the characteristics of the initial study population. Whilst the mean LVEF was 26% it should be remembered that patients were young (mean age 60 years), had predominantly NYHA class II heart failure and low rates of advanced renal disease and prior cerebrovascular accident, and as such may not be representative of a general ischaemic cardiomyopathy population. Subsequently the risk of surgical treatment in a non-study population may differ from that reported in STICHES. Therefore the cardiologist, surgeon and patient should carefully consider the short and long term outcomes of CABG prior to embarking upon surgical revascularisation with regard to each patient’s risk.
Another point of interest will be the role of viability testing in patient selection for surgical treatment. The initial viability sub-study of STICH [6] did not suggest that viability is of use in determining treatment strategy. However STICHES extended follow-up data may also clarify this important issue once presented.
References
- Coronary artery surgery study (CASS): a randomized trial of coronary artery bypass surgery. Quality of life in patients randomly assigned to treatment groups. Circulation, 1983. 68(5): p. 951-60.
- Eleven-year survival in the Veterans Administration randomized trial of coronary bypass surgery for stable angina. The Veterans Administration Coronary Artery Bypass Surgery Cooperative Study Group. N Engl J Med, 1984. 311(21): p. 1333-9.
- Yusuf, S., et al., Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomised trials by the Coronary Artery Bypass Graft Surgery Trialists Collaboration. Lancet, 1994. 344(8922): p. 563-70.
- Velazquez, E.J., et al., Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med, 2011. 364(17): p. 1607-16.
- Velazquez, E.J., et al., Coronary-Artery Bypass Surgery in Patients with Ischemic Cardiomyopathy. N Engl J Med, 2016. 374(16): p. 1511-20.
- Bonow, R.O., et al., Myocardial viability and survival in ischemic left ventricular dysfunction. N Engl J Med, 2011. 364(17): p. 1617-25.
 IASC
IASC 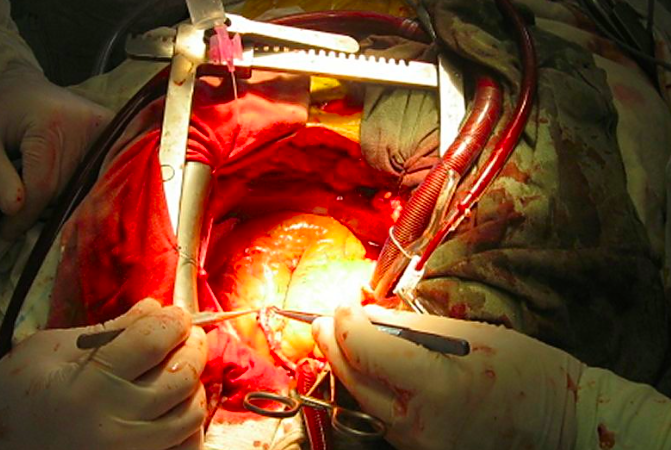



































330 Comments
ANNA
agosto 3, 2021, 10:51 amThanks to God and also to Dr. OBINA, the great herbal man that cured me from HERPES. I contacted the virus from my partner three years ago, i almost spent all i had because i was restless and i need to get rid of the virus and i did not rest until i saw people testimony about Dr. OBINA recommendation online for how he has being curing HERPES with his herbs and i emailed him and tell him my problem and he prepare my cure and send it to me and gave me instructions on how to use the herbs and behold after i finish drinking it i went to the hospital for checkup and the result was negative and the virus was completely gone from my body. You can contact Dr. OBINA to get your herbs too and cure yourself from these virus. His Email: obinnaspelltemple@yahoo.com or add him on WhatsApp +19492293867 Dr. OBINA has cure so many different type of diseases with his herbs such as HERPES, HIV/AIDS. CANCER of all kinds, HSV 1&2, DIABETES and so many more. I want to thank God for using Dr. OBINA to cure me from herpes. Dr. OBINA is truly gifted by God. add him on WhatsApp +19492293867
REPLYMartha Jecorick@ANNA
noviembre 14, 2022, 10:28 pmDR. OSATO`S CURE FOR HERPES1&2 – A NATURAL WAY TO GET HERPES1&2 CURED. If you have been looking for ways to naturally get rid of the herpes simplex virus from your body completely, then you are welcome to read further. Let’s face reality here, you have tried so many counter drugs and you are confused, weak and angry because nothing seems to work. Good News For you my friend…. Yes, I came with good news that will liberate you from the pains and stress of herpes outbreak, you will get total cure from this virus using Dr. Osato Herbal Methodology. Who is Dr. Osato? You may ask. Dr. Osato is a herbalist and a naturalist. He researched and identified some herbs and established a unique methodology to healing the human body using Herbal medicine that was confidently entrenched in his over 30 years of experience. According to him, he has the cure for so many diseases/virus like GENITAL HERPES, HIV, DIABETES, CANCER, HPV, HSV1&2, GENITAL WART, SHINGLES, VAGINAL INFECTION and so many more. You can reach Dr Osato on his email: osatoherbalcure@gmail.com or WhatsApp +2347051705853. You can also contact him through his website: https://osatoherbalcure.wordpress.com I am using this medium to inform everyone how to get treated of herpes using Dr Osato recommended Herbal methodology.
REPLYDiana@Martha Jecorick
agosto 2, 2023, 3:30 amThe best herpes remedy online…
Thank you D Robinson buckler for saving my life,
I am cured from herpes.
He can also restore broken.
Relationship/marriage with spiritual prayer.
He brought my ex lover back.
My ex-lover loves me unconditionally.
Cures the following..
Shingles,
Cold sore,
HPV,
HSV1&2,
Fibroid,
Erectile Dysfunction..
His result is 100% guarantee….
r.buckler11 (@) gmail.. com
REPLYsusan@ANNA
abril 8, 2023, 7:20 amI GOT CURED FROM HERPES VIRUS:
REPLYI’m so Happy to write this article because I know it will help a lot of people who are suffering from Herpes virus . I got positive to the deadly Virus called herpes. and I lost hope completely because I heard there was no cure . I want to thank doctor aba for getting. rid of my herpes with the help of his natural herpes eraser . I used the medicine as he instructed and I got cured after completing the dose of the medicine. It’s really like a dream but I’m so happy that’s the reason why I published this article. contact him for herpes cure or other disease cure via
Email: dr.abaherbalhome@gmail.com.
Diana@ANNA
agosto 2, 2023, 3:30 amThe best herpes remedy online…
Thank you D Robinson buckler for saving my life,
I am cured from herpes.
He can also restore broken.
Relationship/marriage with spiritual prayer.
He brought my ex lover back.
My ex-lover loves me unconditionally.
Cures the following..
Shingles,
Cold sore,
HPV,
HSV1&2,
Fibroid,
Erectile Dysfunction..
His result is 100% guarantee….
r.buckler11 (@) gmail.. com
REPLYLiz@ANNA
septiembre 15, 2023, 12:43 amA client recommended me to contact this herbal Doctor for herpes cure. I purchased the herbal medicine. I followed the instructions on how to use it, after taking the medicine as instructed for 2 weeks, i went for check-up and the result came out negative and i was cured of herpes, I am now free from Herpes. I am still in shock on how this herbal medicine works. You can try and see for yourself, I won’t believe it works if i never gave a try. This is a miracle herbs. You can contact him on his email ………… Robinsonbuckler11@gmail.com
REPLYKATHRINE MELNICK
agosto 8, 2021, 4:11 pmBEST URGENT EFFECTIVE LOVE SPELL TO GET YOUR EX/HUSBAND/WIFE BACK FAST AND TO SAVE YOUR MARRIAGE NOW CONTACT LORD ZULU ON WHATSAPP DIRECTLY +1 (424) 361‑7554. Hi everyone I’m here to testify of a great and powerful spell caster called Lord Zulu. I was so confused and devastated when my husband left me without a word, I needed him back desperately because I loved him so much. So a friend of mine introduced me to this powerful spell caster who had helped her in getting her lover back, so I contacted him and he promised that in less than 72 hours he will come back to me. After I did all he asked, to my greatest surprise my husband who had refused to speak with me came to my house and asked for forgiveness for all he had made me go through and now we are living happily together, if you have any relationship problem I will advise you contact him for your testimonies . Below are his contact details. Contact him on WhatsApp @ +1(424)361‑7554. BLOGSPOT: allsupremepowersolutionhome.blogspot.com EMAIL: Allsupremepowersolutionhome@gmail.com
REPLYKATHRINE MELNICK
agosto 8, 2021, 4:11 pmBEST URGENT EFFECTIVE LOVE SPELL TO GET YOUR EX/HUSBAND/WIFE BACK FAST AND TO SAVE YOUR MARRIAGE NOW CONTACT LORD ZULU ON WHATSAPP DIRECTLY +1 (424) 361‑7554. Hi everyone I’m here to testify of a great and powerful spell caster called Lord Zulu. I was so confused and devastated when my husband left me without a word, I needed him back desperately because I loved him so much. So a friend of mine introduced me to this powerful spell caster who had helped her in getting her lover back, so I contacted him and he promised that in less than 72 hours he will come back to me. After I did all he asked, to my greatest surprise my husband who had refused to speak with me came to my house and asked for forgiveness for all he had made me go through and now we are living happily together, if you have any relationship problem I will advise you contact him for your testimonies . Below are his contact details. Contact him on WhatsApp @ +1(424)361‑7554. BLOGSPOT: allsupremepowersolutionhome.blogspot.com EMAIL: Allsupremepowersolutionhome@gmail.com
REPLYKATHRINE MELNICK
agosto 8, 2021, 4:11 pmBEST URGENT EFFECTIVE LOVE SPELL TO GET YOUR EX/HUSBAND/WIFE BACK FAST AND TO SAVE YOUR MARRIAGE NOW CONTACT LORD ZULU ON WHATSAPP DIRECTLY +1 (424) 361‑7554. Hi everyone I’m here to testify of a great and powerful spell caster called Lord Zulu. I was so confused and devastated when my husband left me without a word, I needed him back desperately because I loved him so much. So a friend of mine introduced me to this powerful spell caster who had helped her in getting her lover back, so I contacted him and he promised that in less than 72 hours he will come back to me. After I did all he asked, to my greatest surprise my husband who had refused to speak with me came to my house and asked for forgiveness for all he had made me go through and now we are living happily together, if you have any relationship problem I will advise you contact him for your testimonies . Below are his contact details. Contact him on WhatsApp @ +1(424)361‑7554. BLOGSPOT: allsupremepowersolutionhome.blogspot.com EMAIL: Allsupremepowersolutionhome@gmail.com
REPLYKATHRINE MELNICK
agosto 8, 2021, 4:11 pmBEST URGENT EFFECTIVE LOVE SPELL TO GET YOUR EX/HUSBAND/WIFE BACK FAST AND TO SAVE YOUR MARRIAGE NOW CONTACT LORD ZULU ON WHATSAPP DIRECTLY +1 (424) 361‑7554. Hi everyone I’m here to testify of a great and powerful spell caster called Lord Zulu. I was so confused and devastated when my husband left me without a word, I needed him back desperately because I loved him so much. So a friend of mine introduced me to this powerful spell caster who had helped her in getting her lover back, so I contacted him and he promised that in less than 72 hours he will come back to me. After I did all he asked, to my greatest surprise my husband who had refused to speak with me came to my house and asked for forgiveness for all he had made me go through and now we are living happily together, if you have any relationship problem I will advise you contact him for your testimonies . Below are his contact details. Contact him on WhatsApp @ +1(424)361‑7554. BLOGSPOT: allsupremepowersolutionhome.blogspot.com EMAIL: Allsupremepowersolutionhome@gmail.com
REPLYmary anne@KATHRINE MELNICK
agosto 27, 2021, 10:46 pmMensaje *
REPLY